Medicare Advantage Crisis: How Transportation Providers Can Turn It Into An Opportunity

The healthcare industry is going through widespread cost pressure. For Medicare Advantage, this means a contraction in enrollment and a reduction in multiple benefits across many plans, specifically medical transportation benefits. The cuts are positioned as an attempt to decrease wasteful spending and improve program integrity, but for passengers, they bring the risk of missed appointments, and for transportation providers, a major loss of revenue. However, in this article, we'll explain why the Medicare Advantage crisis (while potentially painful for many enrollees and providers) represents the biggest market consolidation opportunity in NEMT in over a decade, and how prepared operators can capture significant market share.
Contents:
- Medicare Crisis Explained
- Some Good News: Medicare Cuts Do Not Mean Less Demand for Transportation
- Which Medical Transportation Providers Will Be Affected By The Medicare Cuts?
- Low-Value NEMT Services And Non-Compliance Will Not Be Tolerated
- How NEMT Providers Can Benefit From Medicare Cuts
- Final Thoughts: Medicare Advantage Transportation Is Becoming More Selective, Not Smaller
Medicare Crisis Explained
According to the latest projections, in 2026, Medicare Advantage will be relied upon by 34 million Americans, or 48% of the eligible Medicare population. That level represents a projected decline from prior years and marks the first expected contraction of Medicare Advantage enrollment in nearly two decades. This decline in enrollment is accompanied by a recent pullback in transportation coverage for beneficiaries that is not driven by reduced need. It is driven by financial pressure, utilization trends, and regulatory scrutiny inside Medicare Advantage, not by declining demand for care.
Medicare Advantage plans are adjusting benefits in response to higher-than-expected medical utilization, tighter margins, and ongoing CMS oversight of risk adjustment, documentation, and program integrity. After more than a decade of growth-focused expansion, insurers are now prioritizing profitability over enrollment growth, cutting or decommissioning unprofitable plans. While some federal legislation introduces broader system pressure, transportation benefit reductions are primarily the result of plan-level pricing and compliance dynamics, not a direct statutory elimination of NEMT benefits.
The impact is already visible in states like Maryland, where approximately 100,000 Medicare recipients scrambled to find new health plans by the end of 2025 as insurers fled the state or reduced Medicare Advantage coverage. "We're going to be dealing with the Medicare Advantage issue, which has turned out to be a really big issue for this year," said Maryland Senate Finance Committee Chair Pamela Beidle. The Maryland crisis illustrates how market instability doesn't just affect coverage—it creates operational chaos for providers trying to maintain service networks.
The Maryland crisis isn’t isolated. Nationally, insurers are pulling back MA footprints as profitability tightens. UnitedHealth alone is exiting MA plans in 109 counties for 2026, affecting roughly 180,000 members.
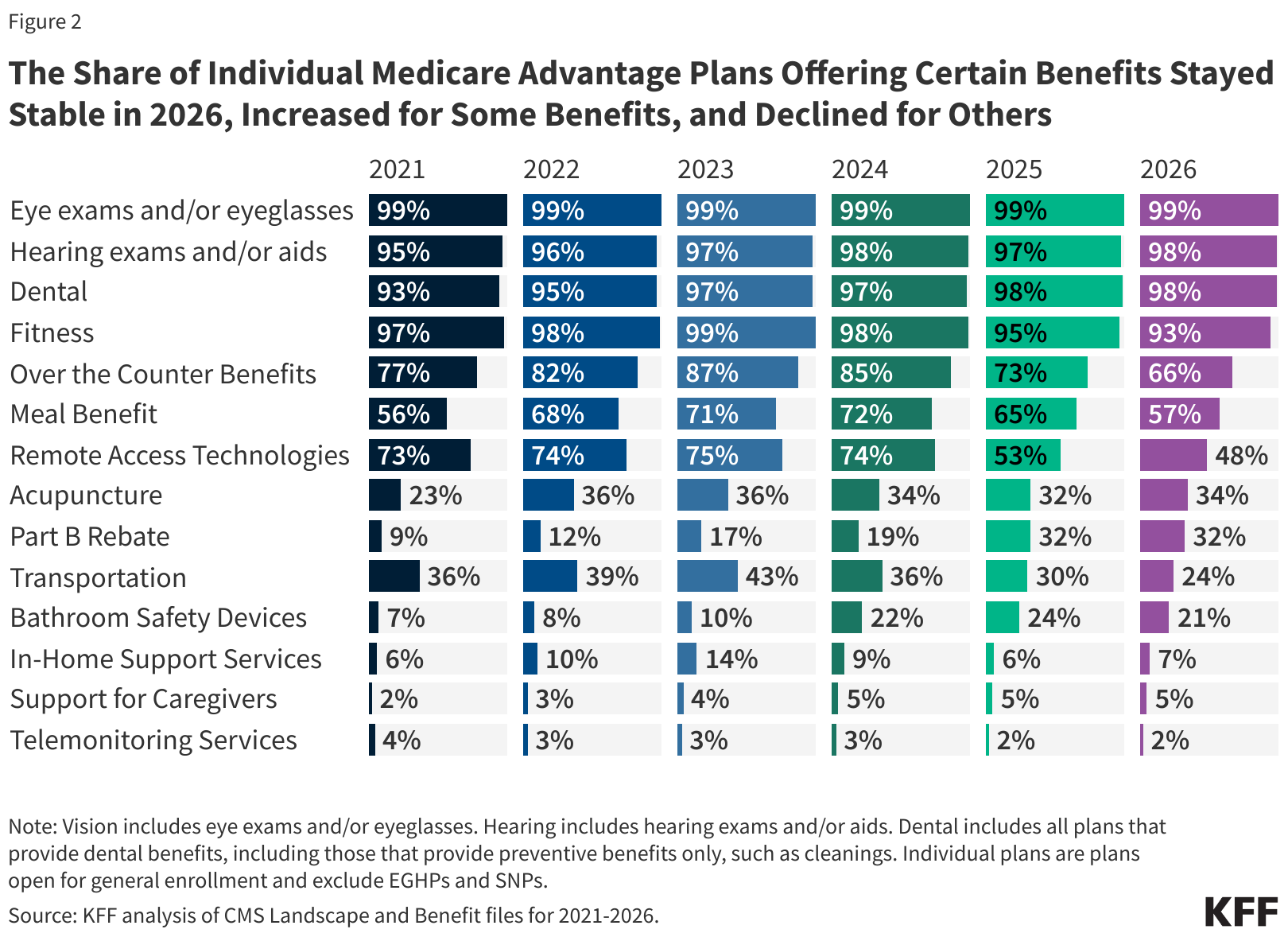
Within the Medicare system, NEMT rides for routine care are largely offered as supplemental benefits in privately run Medicare Advantage Part C. Since the healthcare industry still treats these non-emergency medical transportation rides as non-essential, they are often among the first benefits reduced when insurers attempt to restore margins. In practice, this trend is already visible. According to the Kaiser Family Foundation, the share of individual Medicare Advantage enrollees with transportation benefits has already fallen from 30 percent in 2025 to 24 percent in 2026.
Some Good News: Medicare Cuts Do Not Mean Less Demand for Transportation
Not all news is bad, at least not for all providers. While transportation benefits are shrinking, Medicare Advantage enrollment actually remains robust. The drivers for this market situation are structural: an aging population, higher prevalence of chronic conditions, and sustained preference for managed plans that coordinate care across providers. Solid Medicare Advantage enrollment supports the demand among transportation-eligible members. In fact, Special Needs Plans within Medicare Advantage, which are reserved for higher-acuity enrollees, account for nearly half of recent MA enrollment growth. These plans have much better coverage of transportation for medical needs (67% for SNPs vs 24% for individual plans).
These enrollment patterns change the arithmetic. Even if the cuts lead to a smaller percentage of plans offering transportation benefits, the absolute number of Medicare Advantage members remains large. Moreover, a growing share of transportation demand is concentrated within SNP populations that are more likely to retain transportation benefits in 2026 and beyond. The NEMT market is consolidating around higher-acuity services, including wheelchair transport, bariatric solutions, stretcher services, and dialysis transportation. Eligible medical transportation providers can expect a steady demand for their services; however, the service expectations of the Centers for Medicare & Medicaid Services and Medicare Advantage organizations will become much higher.
Which Medical Transportation Providers Will Be Affected By The Medicare Cuts?
The latest analysis suggests that if medical transportation rides are ambulatory and offered for Medicare members who might be able to find other means of transportation, then they are at major risk of losing coverage. This development exposes providers that primarily offer basic ambulatory rides. A large portion of their business will be increasingly redirected to public transit, paratransit, microtransit, or ridesharing programs.
At the same time, some businesses will be more resilient than others and should be better positioned to weather the storm. The services that are difficult to replace and easier for plans to justify under tighter benefit and audit scrutiny should prevail. Here are some of them:
- Wheelchair-accessible transportation
- Assisted and higher-acuity services, including stretcher van transportation
- Medically supported trips tied to functional limitations
Providers reliant on low-acuity ambulatory volume face a higher risk. Operators offering advanced levels of service are more likely to remain essential as Medicare Advantage applies stricter benefit filters.
Low-Value NEMT Services And Non-Compliance Will Not Be Tolerated
Benefit cuts will likely act as a market filter. Budget pressure will force plans to establish tighter eligibility, more documentation scrutiny, and program integrity checks. These increased expectations will make the following processes unavoidable for all medical transportation companies:
- Driver and vehicle credentialing
- Trip verification and audit trails
- On-time performance and complaint handling
- Documentation quality and billing accuracy
These compliance requirements cannot be satisfied without modern medical transportation software like RouteGenie. Amid Medicare Advantage cuts, providers who stay with manual processes or inadequate NEMT platforms will fail audits and are in danger of being excluded or non-renewed. Importantly, this does not eliminate trips from the system. It redistributes them. Disciplined NEMT providers should treat these financing adjustments not as a crisis but as an opportunity. They can absorb volume from weaker operations and pursue market consolidation.
How NEMT Providers Can Benefit From Medicare Cuts
 This Medicare market realignment is a great opportunity to turn uncertainty into profits; however, only providers who can follow these best practices can successfully do it:
This Medicare market realignment is a great opportunity to turn uncertainty into profits; however, only providers who can follow these best practices can successfully do it:
- Maintain service depth that extends beyond basic ambulatory transport (wheelchair-accessible and stretcher NEMT rides as well as specializations like bariatric transport).
- Pursue the highest operational standards: precise dispatch, on‑time performance, trip verification, and fast complaint/appeals handling.
- Train your staff on HIPAA/PHI safeguards, incident reporting, and other NEMT compliance aspects.
- Maintain high service quality through clearly defined KPIs, corrective actions, continuous improvement, and pursue customer satisfaction. Explore the value-based NEMT model.
- Establish robust credentialing, background checks, vehicle inspections and maintenance protocols.
- Pursue NEMTAC accreditation, which aligns with tightening Medicaid oversight and MA plan quality assurance metrics. Position yourself as a trustworthy go-to provider.
- Collaborate with other providers to form transportation coalitions and win direct contracts. Position yourself as a single regional solution to health systems, MA plans and ACOs.
- Do not turn down transportation requests if your in-house vans are fully booked. You can leverage ridesharing platforms like Uber Health and Lyft Healthcare for ambulatory, low-acuity trips, surge/overflow capacity, long-tail geographies with lots of deadhead miles, and off-peak hours.
Final Thoughts: Medicare Advantage Transportation Is Becoming More Selective, Not Smaller
Let’s sum it up:
- Medicare Advantage transportation is not shrinking uniformly; it is becoming more selective.
- The inflow of enrollees who qualify for transportation benefits can actually offset the cuts and increase the demand for NEMT, not lower it.
- Transportation of higher acuity passengers will be in higher demand in the “post-Medicare cuts environment.”
- Contract volume that will be lost by non-compliant providers can be won by disciplined operations.
Request a RouteGenie demo to meet these higher standards and compete effectively.
About the author

As RouteGenie's Marketing Director, Yurii gained deep knowledge in the NEMT industry. He is an expert in marketing, leveraging all channels to build RouteGenie's brand and ensure NEMT providers have access to powerful NEMT software that can boost their growth. Yurii shares his knowledge by writing content on marketing and healthcare topics, including medical transportation, home care, and medical billing.